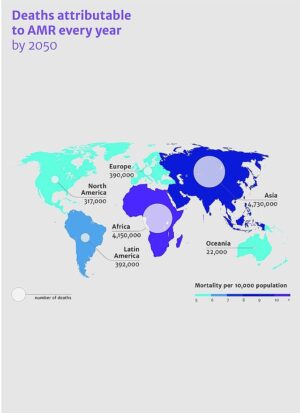
The World Health Organization WHO expects antimicrobial resistance to become a persistent problem. A growing number of people develops resistance against antibiotics. In 2050, this might cause an additional 10 million people to die. What can we do to prevent this?
A major threat
The WHO judges antimicrobial resistance to belong to the top ten threats to public health. The main cause for this is the faulty or overzealous use of antibiotics. To which we can add the lack of clean drinking water and living in unhygienic conditions. WHO judges antimicrobial resistance to come at a high cost. Not just because it will lead to deaths and permanent injury, but also through the cost of caring for the sick and disabled. And yet, we need antibiotics. Much of the success of modern medicine is based on their use; on top of that, consider the use of these medicines at surgery and in chemotherapy.
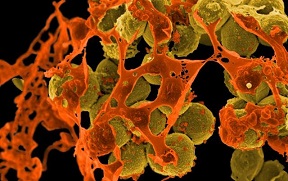
Antimicrobial resistance means that pathogens are no longer vulnerable to the medicines with which we try to control them. This holds not just for bacteria, but also for viruses, moulds and parasites. In case of resistance, we will no longer be able to cure someone infected with the pathogen. This problem doesn’t just occur with respect to humans, it also occurs in animals like cows. And there is bacterial transfer, possibly of resistant specimens, between people and also between people and animals.
Resistance on the rise
An important driver of growing antimicrobial resistance is the way in which we use antibiotics. There is much unnecessary use and overuse, an important factor causing resistance in pathogens. If this happens, people who suffer from certain infections have a hard time controlling them. Well-known conditions in which this occurs are infections of the urinary tract and sex organs, sepsis and some forms of diarrhoea. Some resistant bacteria (Klebsiella pneumoniae and MRSA) have developed so far that we just have one single medicine left that will control them. Other forms of resistance exist as well. As an example, we can often no longer treat parasites that transfer malaria.
Many people seem to think that this problem will rank high on research agendas. But then, they are wrong, says Oscar Kuipers, a University of Groningen professor, to the Dutch magazine De Onderzoeker. Pharmaceutical companies perceive to little earning power in tackling this problem. That’s why the pipeline of new antibiotics dries down more and more. Whereas research into antibiotics takes a lot of time and is beset with disappointments. Some substances do have an antibacterial activity but are too poisonous. And by now, research into new antibiotics has become such a wide-spread field that many disciplines are involved; from chemists and biotechnologists to pharmacists and medical doctors.
Against antimicrobial resistance
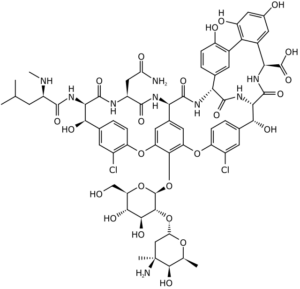
In the Netherlands this led to the erection of NACTAR in 2016 (Novel Antibacterial Compounds and Therapies Antagonizing Resistance). This program has now developed so far that a number of possible medicines has been developed. The next step is organizing preclinical tests. Among the substances to be tested is a variant of the antibiotic vancomycin, that causes growing resistance. The new variant is both more powerful, and active against resistant bacteria.
But the road towards actual industrial production of such a compound is long. Firstly, the safety of the medicine needs to be proven. Then humane testing follows. Within three years, if all goes well. But there is no alternative. We cannot leave the problem of antimicrobial resistance to the market to solve – for it will do not much about it. The pathway of substances against antimicrobial resistance is long.
A new approach
Not just humane health is at stake. In the veterinary realm, similar problems have surfaced. Loss of trust in health care as such may surface, says the site health.belgium.be. Particularly, if resistant bacteria would spread in hospitals or through the food chain. And then we don’t even mention the cost involved. Solving this problem will not be easy. And more problematic as we need to have an eye on animal husbandry as well.
Interesting? Then also read:
Chemistry vs. bacteria, # 50. Resistance, a second look
Chemistry vs. bacteria, # 66. The evolutionary arms race
Antibiotics resistance, do ants have the solution?
